Sepsis is a serious and potentially life-threatening condition that occurs when the body’s response to an infection becomes dysregulated. In children, sepsis can develop quickly and lead to severe complications. The ability to identify the signs and symptoms of sepsis early is crucial to ensure timely intervention and improve outcomes.
In this blog, we will explore what sepsis is, how it develops in children, its symptoms, risk factors, and treatment options.
What is Sepsis?
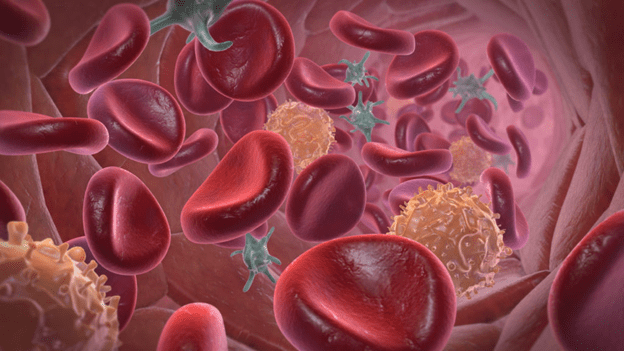
Sepsis occurs when the body’s immune system responds to an infection in an exaggerated or uncontrolled manner. Normally, the body fights off infections using immune responses that include inflammation. However, in sepsis, the inflammation becomes widespread and can affect multiple organs. This systemic response can lead to tissue damage, organ failure, and in severe cases, death.
While sepsis can affect anyone, children are particularly vulnerable. Infants, young children, and those with weakened immune systems or chronic conditions are at higher risk.
How Does Sepsis Develop in Children?
Sepsis can develop in children when a bacterial, viral, or fungal infection in the body spreads. It typically starts with a localized infection in areas like the lungs (pneumonia), urinary tract, skin (cellulitis), or gastrointestinal system. In some cases, the infection may be difficult to pinpoint, and the child may appear to have a general illness.
Sepsis develops when the infection triggers an overwhelming immune response, leading to widespread inflammation. This inflammation can cause a cascade of changes in the body, including:
- Impaired blood flow: Blood vessels may dilate and leak fluid, leading to low blood pressure (shock).
- Organ dysfunction: Decreased oxygen delivery and nutrient supply can lead to organ failure, especially in vital organs like the heart, kidneys, and lungs.
- Blood clotting abnormalities: In some cases, the immune system’s response can trigger abnormal clotting, which can damage blood vessels and organs.
Symptoms of Sepsis in Children
Sepsis can develop rapidly, and recognizing the signs early can make a significant difference in the outcome. The symptoms of sepsis can vary depending on the age of the child and the severity of the infection, but common signs to watch for include:
- Fever or Hypothermia: A high fever is often one of the first signs of infection, but in some cases, sepsis can cause the body temperature to drop below normal (hypothermia), especially in newborns and young children.
- Rapid Breathing or Difficulty Breathing: Sepsis can cause the child to breathe more quickly than usual or even struggle to breathe. They may also have bluish skin around the lips, fingers, or toes due to lack of oxygen.
- Fast Heart Rate: The body tries to compensate for the drop in blood pressure by increasing the heart rate. A significantly fast heart rate is a red flag in children with suspected sepsis.
- Low Blood Pressure (Shock): As the infection spreads, the child’s blood pressure may drop dangerously low. This can lead to symptoms like dizziness, weakness, confusion, or a feeling of fainting.
- Poor Feeding or Difficulty Eating: Especially in infants and young children, sepsis can cause lethargy, difficulty feeding, or loss of appetite.
- Cold, Clammy Skin: As blood flow is redirected to vital organs, the skin can feel cold, pale, and clammy to the touch. This may be a sign that the child’s body is not receiving enough blood.
- Confusion or Disorientation: In severe cases of sepsis, children may become confused, disoriented, or unresponsive. They may seem unusually sleepy or difficult to wake up.
- Abnormal Skin Rashes: Sepsis can sometimes cause a rash or purple spots on the skin (petechiae), which are a result of blood vessels leaking due to impaired clotting.
- Decreased Urine Output: When the kidneys are affected by sepsis, urine output can decrease, and the child may produce very little or no urine at all.
Risk Factors for Sepsis in Children
Certain factors can increase a child’s risk of developing sepsis. These include:
- Age: Infants and very young children are more susceptible to infections and sepsis. Their immune systems are still developing, making it harder for them to fight infections.
- Weakened Immune System: Children with compromised immune systems due to conditions like cancer, organ transplants, or immunodeficiencies are at higher risk for infections that can lead to sepsis.
- Chronic Health Conditions: Children with chronic illnesses such as diabetes, heart disease, or respiratory conditions may be more prone to infections and sepsis.
- Invasive Medical Procedures: Children who have had surgery, central lines (for feeding or IV access), or urinary catheters are at greater risk for infections that can lead to sepsis.
- Premature Birth: Premature infants have an underdeveloped immune system and are at a higher risk of infections that can lead to sepsis.
- Previous Infections: If a child has a history of frequent infections, including ear infections, pneumonia, or urinary tract infections, they may be at an increased risk for developing sepsis.
Diagnosis of Sepsis in Children
When sepsis is suspected, quick action is necessary to confirm the diagnosis and initiate treatment. Doctors typically perform a physical examination and may order several tests, including:
- Blood Cultures: To identify the specific bacteria or virus causing the infection.
- Complete Blood Count (CBC): To check for signs of infection and inflammation, such as elevated white blood cell counts.
- Urine Tests: To detect urinary tract infections that may have led to sepsis.
- Chest X-ray or Ultrasound: To check for lung infections (like pneumonia) or other sources of infection in the body.
- Other Cultures: Cultures of wounds, the throat, or other bodily fluids may also be taken to identify the pathogen.
Early diagnosis and intervention are key to reducing the risk of severe complications and death from sepsis.
Treatment of Sepsis in Children
Treatment for sepsis typically begins immediately after the diagnosis is confirmed, as the condition can progress quickly. The main goals of treatment are to:
- Control the Infection: Antibiotics or antifungal medications are typically administered intravenously (IV) to treat the underlying infection. If the infection is viral, antiviral medications may be given.
- Stabilize Vital Functions: Sepsis can lead to life-threatening changes in heart rate, blood pressure, and breathing. Children may need oxygen, intravenous fluids, or medications to support these vital functions.
- Monitor Organ Function: Organ support may be required if the kidneys, heart, or lungs are affected. In some cases, a ventilator may be necessary to help with breathing.
- Surgery (if needed): In cases where there is a localized infection (e.g., an abscess), surgery may be required to drain the infection and remove infected tissue.
- Supportive Care: In severe cases of sepsis, children may need to be placed in a pediatric intensive care unit (PICU) for close monitoring and treatment.
Prevention of Sepsis in Children
While not all cases of sepsis can be prevented, there are steps that can reduce a child’s risk of developing sepsis:
- Timely Vaccination: Ensure that children are up to date on vaccinations to protect them from infections like pneumonia, meningitis, and influenza, which can lead to sepsis.
- Prompt Treatment of Infections: Seek medical attention if a child shows signs of an infection, especially if they develop a fever, are unusually sleepy, or show other warning signs.
- Good Hygiene Practices: Encourage regular handwashing to prevent the spread of infections and minimize the risk of bacterial or viral illnesses.
- Careful Monitoring in High-Risk Children: Children with chronic health conditions or those recovering from surgery should be closely monitored for signs of infection.
Conclusion
Sepsis is a serious and potentially life-threatening condition that requires immediate attention, especially in children. Understanding the symptoms, risk factors, and treatment options for sepsis can help ensure a timely response and improve outcomes for affected children. Early recognition and prompt medical intervention are key to managing sepsis and reducing its severe complications.
If you suspect that your child may be developing sepsis, seek emergency medical care immediately to ensure the best chance of recovery.
Consult us today at Bluebird Children’s Hospital for expert care!